O diabetes mellitus como fator imunossupressor predisponente da mucormicose: um relato de caso
##plugins.themes.bootstrap3.article.main##
Resumo
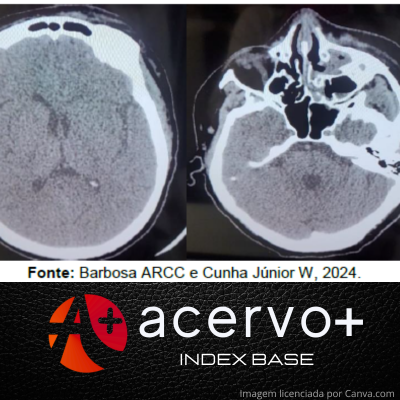
Objetivo: Relatar um estudo de caso de mucormicose em uma paciente diabética com diagnóstico tardio e consequente evolução desfavorável. Detalhamento do caso: Paciente do sexo feminino, 48 anos de idade, hipertensa, diabética, dislipidêmica e obesa. Inicialmente com quadro inespecífico de cefaleia e dor na cavidade oral, passou por atendimento com dentista que fez diagnóstico errôneo de infecção dentária, sendo iniciado amoxicilina com clavulanato. Porém, após alguns dias evoluiu com piora clínica, buscando atendimento médico. Já se apresentava com quadro avançado e sinais de infecção sistêmica, sendo então, encaminhada para leito de terapia intensiva, onde foi aventada hipótese de infecção fúngica. Devido gravidade e extensão da doença foi optado não realizar abordagem cirúrgica, mantendo-se apenas o tratamento medicamentoso. Após alguns dias paciente evoluiu a óbito. Considerações finais: A mucormicose é uma doença grave e potencialmente fatal. É uma infecção oportunista, estando no grupo principal, os portadores de diabetes mellitus descompensado. O diagnóstico exige um alto índice de suspeição e início imediato do tratamento, pois o atraso no diagnóstico acarreta evolução desfavorável.
##plugins.themes.bootstrap3.article.details##
Copyright © | Todos os direitos reservados.
A revista detém os direitos autorais exclusivos de publicação deste artigo nos termos da lei 9610/98.
Reprodução parcial
É livre o uso de partes do texto, figuras e questionário do artigo, sendo obrigatória a citação dos autores e revista.
Reprodução total
É expressamente proibida, devendo ser autorizada pela revista.
Referências
2. BRUNET K e RAMMAERT B. Mucormycosis treatment: Recommendations, latest advances, and perspectives. Journal de Mucologie Medicale, 2020; 30 (3): 101007.
3. CHIKLEY A, et al. Mucormycosis of the Central Nervous System. Journal of Fungi, 2019; 5(3): 59.
4. CORNELLY OA, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. The Lancet.Infectious diseases, 2019; 19 (12): 405-421.
5. DARWISH RM, et al. Mucormycosis: The hidden and forgotten disease. Journal of applied microbiology, 2022; 132(6): 4042-4057.
6. FATHIMA AS, et al. Mucormycosis: A triple burden in patients with diabetes during COVID-19 Pandemic. Health Sciences Review. Health Sci Rev (Oxf), 2021; 1(3): 100005.
7. FERNADES KT e BASTOS ASM. Mucormicose em pacientes portadores de diabetes mellitus: uma revisão de literatura. Revista Ibero-Americana de Humanidades, Ciências e Educação, 2022; 8 (8): 398-404..
8. GUAN WJ, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. The Journal of Emergency Medicine, 2020; 58(4): 711-712.
9. HASSAN MIA e VOIGT K. Pathogenicity patterns of mucormycosis: epidemiology, interaction with immune cells and virulence factors. Medical Mycology, 2019; 57 (2): 245–256.
10. HERRERA EM, et al. Mucormicose rinocerebral em alta? O impacto da epidemia mundial de diabetes. Anais Brasileiros de Dermatologia, 2021; 96 (2): 196 -199.
11. VASUDEVAN B, et al. Mucormycosis: the scathing invader. Indian Journal of Dermatology, 2021; 66 (4): 393-400.
12. MINISTÉRIO DA SAÚDE. Mucormicose (fungo negro). 2021. Disponível em: https://www.gov.br/saude/pt-br/assuntos/saude-de-a-a-z/m/mucormicose. Acessado em: 01 de dezembro de 2023.
13. PAI V, et al. Rhino-orbito-cerebral Mucormycosis: Pictorial Review. Insights into Imaging, 2021; 12 (1): 167.
14. REID G, et al. Mucormycosis. Seminars in respirator and critical care medicine, 2020; 41 (1): 99-114.
15. SKIADA A, et al. Epidemiology and diagnosis of mucormycosis: an update. Journal of fungi, 2020; 6 (4): 265.
16. SMITH C e LEE SC. Current treatments against mucormycosis and future directions. PLoS Pathogens, 2022; 18 (10): 1010858.
17. STEINBRINK JM e MICELI MH. Mucormycosis. Infectious Disease Clinics of North America, 2021; 35 (2): 435–452.