Síndrome de Ativação Macrofágica secundária a Doença de Still
##plugins.themes.bootstrap3.article.main##
Resumo
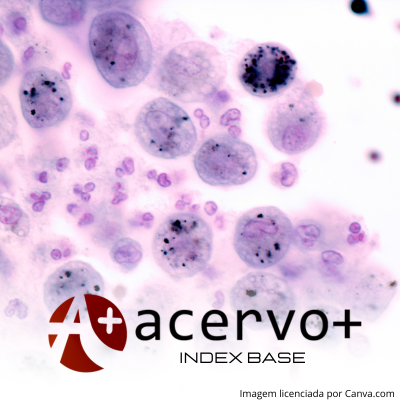
Objetivo: relatar o caso de uma paciente hospitalizada com diagnóstico de Doença de Still e Síndrome de Ativação Macrofágica. Detalhamento de caso: Paciente do sexo feminino, 17 anos, negra, admitida na enfermaria de Clínica médica com relato de dor na garganta, oligoartrite, febre recorrente com média de 38,5 °C, manchas hipercrômicas pruriginosas em dorso, membros superiores e abdome que pioravam com pico febril há cerca de 30 dias, evoluindo durante internação com crise convulsiva seguida de sonolência, letargia, com resposta apenas aos estímulos dolorosos e hipotensão. No décimo dia de internação a paciente apresentou hepatoesplenomegalia ao exame físico, sem outras alterações significativas e queixa de amnesia retrógrada. Os exames laboratoriais constavam anemia, plaquetopenia, aumento de transaminases, hipertrigliceridemia, aumento de ferritina sérica e fibrinogênio no valor de 150, preenchendo 5 dos 9 critérios para diagnóstico de Síndrome da Ativação Macrofágica (SAM). Considerações finais: A doença de Still e a Síndrome de ativação Macrofágica são doenças raras, que implicam grande morbimortalidade na vida dos pacientes acometidos e são primariamente diagnósticos de exclusão. Este trabalho demonstra que o diagnóstico de Síndromes febris pode ser um desafio e reitera a importância da qualidade da assistência.
##plugins.themes.bootstrap3.article.details##
Copyright © | Todos os direitos reservados.
A revista detém os direitos autorais exclusivos de publicação deste artigo nos termos da lei 9610/98.
Reprodução parcial
É livre o uso de partes do texto, figuras e questionário do artigo, sendo obrigatória a citação dos autores e revista.
Reprodução total
É expressamente proibida, devendo ser autorizada pela revista.
Referências
2. ARINGER M, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Annals of the Rheumatic Diseases, 2019; 78(9): 1151–1159.
3. CARVALHO FILHO AX, et al. Síndrome de Ativação Macrofágica Secundária à Infecção Aguda Pelo Vírus Epstein-Barr. Rev Bras Reumatol, 2008; 48(3): 179–183.
4. ELOSEILY EMA, et al. Ferritin to Erythrocyte Sedimentation Rate Ratio: Simple Measure to Identify Macrophage Activation Syndrome in Systemic Juvenile Idiopathic Arthritis. ACR Open Rheumatology, 2019; 1(6): 345–349.
5. GERFAUD-VALENTIN M, et al. Adult-onset Still’s disease. Autoimmunity Reviews, 2014; 13: 708-722.
6. GERFAUD-VALENTIN M, et al. Adult-onset still disease: Manifestations, treatment, outcome, and prognostic factors in 57 patients. Medicine, 2014b; 93(2): 91-99.
7. GIACOMELLI R, et al. A comprehensive review on adult onset Still’s disease. Journal of Autoimmunity, 2018; 93: 24-36.
8. JORDAN MB, et al. How I treat hemophagocytic lymphohistiocytosis. Blood, 2011; 118(15): 4041–4052.
9. JORDAN MB, et al. Challenges in the diagnosis of hemophagocytic lymphohistiocytosis: Recommendations from the North American Consortium for Histiocytosis (NACHO). Pediatric Blood and Cancer, 2019; 66(11).
10. LAURENT C, et al. Journal of clinical oncology Impact of Expert Pathologic Review of Lymphoma Diagnosis: Study of Patients from the French Lymphopath Network. J Clin Oncol., 2010; 35: 2008–2017.
11. LERKVALEEKUL B e VILAIYUK S. Macrophage activation syndrome: Early diagnosis is key. Open Access Rheumatology: Research and Reviews, 2018; 39: 2379-2386.
12. LIGHTFOOT JR, et al. The American college of rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis & Rheumatism,1990; 33(8): 1088–1093.
13. MAGADUR-JOLY G, et al. Epidemiology of adult Still’s disease: Estimate of the incidence by a retrospective study in West France. Annals of the Rheumatic Diseases, 1995; 54(7): 587–590.
14. MAGALHÃES R. Síndrome da Ativação Macrofágiaca. Dissertação (Mestrado Integrado em medicina), Faculdade de Medicina de Lisboa, Universidade de Lisboa, Lisboa, 2019; 46p.
15. MARKS M e MARKS JL. Viral arthritis. Clin Med(Lond), 2016; 16(2): 129–134.
16. MINOIA F, et al. Clinical features, treatment, and outcome of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: A multinational, multicenter study of 362 patients. Arthritis and Rheumatology, 2014; 66(11): 3160–3169.
17. MONGE P, et al. Pan-American League of Associations for Rheumatology-Central American, Caribbean and Andean Rheumatology Association Consensus-Conference Endorsements and Recommendations on the Diagnosis and Treatment of Chikungunya-Related Inflammatory Arthropathies in Latin America. Journal of Clinical Rheumatology, 2019; 25(2): 101–107.
18. NIGROVIC PA, et al. Review: Genetics and the Classification of Arthritis in Adults and Children. Arthritis and Rheumatology, 2018; 70(1): 7-17.
19. SANCHES BERTUCCI F, et al. Doença de Still do adulto: um desafio diagnóstico. Rev Soc Bras Clin Med., 2020; 18(2): 87-90.
20. SCHULERT GS, et al. Effect of Biologic Therapy on Clinical and Laboratory Features of Macrophage Activation Syndrome Associated with Systemic Juvenile Idiopathic Arthritis. Arthritis Care & Research, 2018; 70(3): 409–419.
21. SHIGA T, et al. Usefulness of Interleukin-18 as a Diagnostic Biomarker to Differentiate Adult-Onset Still’s Disease With/Without Macrophage Activation Syndrome From Other Secondary Hemophagocytic Lymphohistiocytosis in Adults. Frontiers in Immunology, 2021; 12: 1-11.
22. STILL GF. On a form of chronic joint disease in children. Archives of Disease in Childhood, 1941; 16(87): 156–165.
23. WANG A, et al. Management considerations in infective endocarditis: A review. JAMA - Journal of the American Medical Association, 2018; 320(1): 72-83.
24. WANG R, et al. Macrophage activation syndrome associated with adult-onset Still’s disease: a multicenter retrospective analysis. Clinical Rheumatology, 2020; 39(8): 2379–2386.
25. YAMAGUCHI M, et al. Preliminary criteria for classification of adult Still’s disease. The Journal of rheumatology, 1992; 19(3): 424—430.