Análise epidemiológica das neoplasias de esôfago na região sudeste do Brasil entre 2011 a 2021
##plugins.themes.bootstrap3.article.main##
Resumo
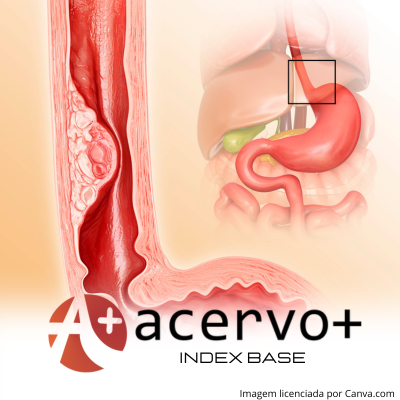
Objetivo: Descrever a análise epidemiológica das neoplasias de esôfago na região sudeste do Brasil no período de 2011 a 2021. Métodos: Trata-se de um estudo epidemiológico do tipo ecológico com coleta de dados realizada no Departamento de Informática do SUS (DATASUS) através do Sistema de Informações de Câncer (SISCAN - câncer de esôfago). A população foi composta por todos os casos notificados de Neoplasias Malignas de Esôfago na região Sudeste do Brasil no período, imputados no tabulador genérico de domínio público (Tabnet), pela Classificação Internacional de Doenças (CID) C15. Utilizou-se variáveis como estado, sexo, faixa etária e ano. A busca foi realizada em novembro de 2023. Resultados: A taxa de mortalidade apresentou queda a partir de 2018, sendo maior no sexo masculino e nas faixas etárias a partir dos 50 anos. A incidência se mantém linear, com discreta redução de 2016 adiante. Foram observadas altas taxas de letalidade no intervalo, evidenciando a gravidade dessa doença. Conclusão: São necessários mais estudos para a compreensão dos fatores que levam a resistir às altas taxas de incidência e letalidade dessa neoplasia na região sudeste do Brasil, com o intuito de diagnosticar e tratar precocemente.
##plugins.themes.bootstrap3.article.details##
Copyright © | Todos os direitos reservados.
A revista detém os direitos autorais exclusivos de publicação deste artigo nos termos da lei 9610/98.
Reprodução parcial
É livre o uso de partes do texto, figuras e questionário do artigo, sendo obrigatória a citação dos autores e revista.
Reprodução total
É expressamente proibida, devendo ser autorizada pela revista.
Referências
2. BRASIL. Ministério da Saúde. DATASUS. Tabnet. Brasília, DF: Ministério da Saúde, 2023. Disponível em: https://datasus.saude.gov.br/mortalidade-desde-1996-pela-cid-10v. Acessado em: 19 novembro de 2023.
3. BRASIL. Ministério da Saúde. Vigitel Brasil 2006-2011. Estimativas sobre a frequência e distribuição sociodemográfica de tabagismo e consumo abusivo de álcool nas capitais dos 26 estados brasileiros e no distrito federal entre 2006 e 2020. Brasília: Ministério da Saúde; 2022. Disponível em: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/svsa/vigitel/vigitel-brasil-2006-2020-e-tabagismo-e-consumo-abusivo-de-alcool.pdf. Acessado em: 24 novembro de 2023.
4. CRUZ AIBM, et al. Perfil dos Pacientes com Câncer de Esôfago Diagnosticados entre 2001 e 2010 no Brasil. Revista Brasileira de Cancerologia, 2018; 64(4): 471-477.
5. DERAKHSHAN, MH, et al. Worldwide inverse association between gastric cancer and esophageal adenocarcinoma suggesting a common environmental factor exerting opposing effects. The American journal of gastroenterology, 2016; 111(2), 228-239.
6. DONG J, et al. Sex-Specific Genetic Associations for Barrett’s Esophagus and Esophageal Adenocarcinoma. Gastroenterology, 2020; 159:2065–2076.
7. FARINATTI PTV. Teorias biológicas do envelhecimento: do genético ao estocástico. Revista Brasileira De Medicina Do Esporte, 2002; 8(4): 129–138.
8. GIMENO SGA, et al. Fatores de risco para o câncer de esôfago: estudo caso-controle em área metropolitana da região Sudeste do Brasil. Revista Saúde, 1995; 29(3): 159-165.
9. HAMEL C, et al. Screening for esophageal adenocarcinoma and precancerous conditions (dysplasia and Barrett’s esophagus) in patients with chronic gastroesophageal reflux disease with or without other risk factors: two systematic reviews and one overview of reviews to inform a guideline of the Canadian Task Force on Preventive Health Care (CTFPHC). Systematic Reviews, 2020; 9:20; 2.
10. HENRY MACA, et al. Esophageal cancer in patient with chagasic megaesophagus. Arq Gastroenterol. 2007; 44(2): 151-155.
11. INCA. Instituto Nacional de Câncer. Câncer de esôfago. 2022. Disponível em
12. INCA. Instituto Nacional de Câncer. Estimativa de 2023. Disponível em https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/estimativa-2023.pdf. Acessado em: 15 de novembro de 2023.
13. IBGE. Instituto Brasileiro de Geografia e Estatística. Censo Brasileiro de 2022. Disponível em https://agenciadenoticias.ibge.gov.br/agencia-noticias/2012-agencia-de-noticias/noticias/37237-de-2010-a-2022-populacao-brasileira-cresce-6-5-e-chega-a-203-1-milhoes. Acessado em: 15 de novembro de 2023.
14. KUIAVA VA, et al. Epidemiological profile of esophageal cancer mortality in Rio Grande do Sul and its health regions. Revista Clinical & Biomedical Research. 2018; 38(3): 213-217.
15. LAGERGREN J, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. New England journal of medicine, 1999; 340(11): 825-831.
16. MENEZES AM, et al. Risco de câncer de pulmão, laringe e esôfago atribuível ao fumo. Revista Saúde Pública. 2002; 36(2): 129-34.
17. QUEIROGA RC. Câncer de esôfago: epidemiologia, diagnóstico e tratamento. Revista Brasileira Cancerologia. 2006; 52(2): 173-178.
18. RIBEIRO LCB. Comparação entre as modalidades de tratamento do câncer de esôfago e da junção esofagogástrica no Instituto Nacional de Câncer - Brasil: um estudo observacional retrospectivo. Dissertação (Mestrado em Oncologia) – Instituto Nacional de Câncer José Alencar Gomes da Silva, Rio de Janeiro, 2019; 118p.
19. STROBE. 2023. Strengthening the reporting of observational studies in epidemiology. Disponível em: https://www.strobe-statement.org. Acesso em: 15 de novembro de 2023.
20. THULER FP, et al. Neoplasia avançada de esôfago: diagnóstico ainda muito tardio. Arq Gastroenterol. 2006; 43(3): 206–211.
21. XU Q, et al. The treatments and postoperative complications of esophageal cancer: a review. Journal of Cardiothoracic Surgery. 2020; 15:163; 2-4.